With small bumps on your forehead or cheeks, I find they most commonly arise from clogged pores, acne, milia, or allergic reactions, though they can also indicate infection or dermatitis requiring medical care; I assess appearance, duration and triggers to guide whether simple at-home care, topical treatments, or seeing a clinician is best, and I emphasize that many bumps are treatable and preventable with proper cleansing, sun protection and avoiding irritants.
Key Takeaways:
- Acne (whiteheads, blackheads, closed comedones) from excess oil, clogged pores, bacteria, or hormones.
- Milia-tiny white keratin-filled cysts that form under the skin and don’t pop like pimples.
- Contact dermatitis or irritation from skincare, hair products, makeup, fragrances, or sweat.
- Rosacea or perioral dermatitis causing small red papules with flushing or persistent irritation.
- Folliculitis or heat rash when hair follicles or sweat ducts become blocked or infected.
- Benign growths such as sebaceous hyperplasia or keratin cysts that mimic small bumps and persist.
- See a dermatologist for sudden onset, painful, spreading, bleeding, or treatment-resistant bumps.
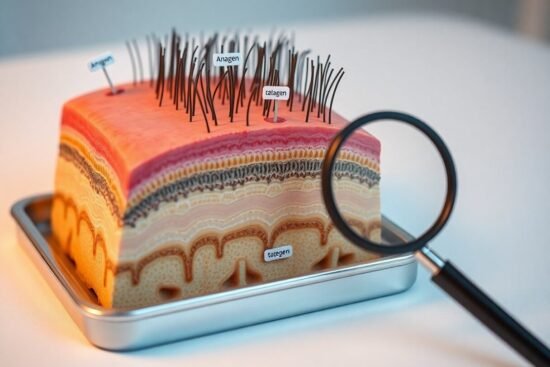
Understanding Skin Bumps
I sort bumps by their origin: clogged pores, trapped keratin, inflamed hair follicles, or minor infections; each presents differently on your forehead or cheeks. In clinical series, acne dominates adolescents while milia and sebaceous changes appear more in adults; timing, texture, and whether lesions are painful help me distinguish them quickly.
Definition of Skin Bumps
A skin bump is any raised lesion from 1 mm to several centimeters that alters texture or color of your skin; it can be soft, firm, movable, or fixed. I look for signs like central plugs, white keratin dots, or warmth to tell if a bump is a comedone, cyst, or inflamed nodule.
Common Types of Bumps
Typical culprits on forehead and cheeks include whiteheads and blackheads (comedones), tiny milia, sebaceous hyperplasia, and inflamed cystic acne; folliculitis and contact papules also appear. I use size, number, and response to squeezing to narrow the diagnosis.
- Whiteheads – closed comedones, often multiple.
- Blackheads – open comedones with dark centers.
- Milia – 1-2 mm pearly keratin cysts.
- Cystic acne – painful, deeper nodules with scarring risk.
- Any persistent or expanding bump lasting over 6 weeks should prompt evaluation.
| Whitehead | Small, closed, flesh-colored; common on cheeks/forehead. |
| Blackhead | Open pore with oxidized surface; not inflamed initially. |
| Milia | 1-2 mm, pearly, keratin-filled, often periorbital or cheeks. |
| Sebaceous hyperplasia | Yellowish papule with central dell, seen in adults. |
| Cyst / Nodule | Larger, tender, risk of scarring if inflamed. |
In practice I find treatment urgency varies: comedonal acne often improves with topical retinoids within 8-12 weeks, while cystic lesions may need oral therapy or drainage; milia often resolve or are extracted in-office under sterile technique. I advise follow-up if lesions change, increase pain, or bleed.
- Topical retinoids – normalize follicular turnover.
- Benzoyl peroxide – reduces surface bacteria and inflammation.
- Extraction – for milia or closed comedones by a clinician.
- Oral antibiotics/Isotretinoin – for moderate to severe inflammatory disease.
- Any worsening rash, fever, or rapidly enlarging nodule warrants immediate care.
| Type | Typical management |
| Whiteheads/Blackheads | Topical retinoid ± chemical exfoliant; avoid picking. |
| Milia | Office extraction or topical retinoid for prevention. |
| Sebaceous hyperplasia | Electrosurgery, cryotherapy, or laser removal if cosmetic concern. |
| Cystic acne | Oral therapy (antibiotics, hormonal, or isotretinoin) and procedural drainage. |
Causes of Bumps on the Forehead and Cheeks
I break causes into four overlapping mechanisms: excess sebum and clogged pores, trapped keratin (milia), immune-driven reactions like allergies or rosacea, and infectious causes (molluscum, fungal). Puberty pushes sebum up-about 85% of adolescents get acne-and persistent inflammatory lesions (especially cysts) can lead to permanent scarring, so I focus on identifying the mechanism quickly to guide treatment.
Acne and Its Variants
I distinguish comedonal acne (whiteheads/blackheads), inflammatory papules/pustules, and deeper cystic or nodular acne; hormones, diet, and medications can all worsen it. Topical retinoids and benzoyl peroxide work well for comedones, while cystic acne often needs systemic therapy-sometimes isotretinoin-with monitoring because of its serious side effects.
Allergic Reactions
Allergic contact dermatitis typically causes itchy, red bumps or tiny blisters on the forehead and cheeks after a new cream, fragrance, sunscreen, or hair product; onset ranges from hours to days. If you develop widespread swelling, difficulty breathing, or rapidly spreading rash, seek urgent care; otherwise I usually recommend stopping the suspect product and considering patch testing.
In practice I separate irritant (non‑immune) from allergic (immune‑mediated) dermatitis by timing and distribution: irritant issues often appear within minutes and at contact sites, while allergic reactions can spread beyond the contact area after 24-72 hours. Common culprits I see are fragrances, preservatives like methylisothiazolinone, nickel from hair clips, and topical antibiotics (neomycin). Management starts with elimination, short courses of topical corticosteroids and oral antihistamines for itch, and referral for patch testing if lesions persist-patch testing identifies the responsible allergen in a high percentage of persistent cases and helps you avoid repeat exposures.
Other Potential Causes
I also consider several less-common culprits that mimic small bumps: viral warts from specific HPV strains, bacterial folliculitis (often Staph aureus), contact dermatitis from fragrances or metals, and tiny syringomas. Warts and folliculitis can be contagious or infected, so I advise prompt evaluation if lesions spread or hurt. Many of these have distinct clues-timing after a new product, clustered follicular papules, or a firm verrucous surface-that help me narrow the diagnosis quickly.
Milia
Milia are 1-2 mm firm, pearly keratin cysts that I often see after skin trauma, heavy creams, or in newborns; they form when keratin gets trapped beneath the epidermis. They’re generally benign and usually resolve spontaneously, but if they persist I recommend professional extraction rather than squeezing because improper removal raises the risk of scarring or infection.
Keratosis Pilaris
Keratosis pilaris presents as rough, sandpaper-like bumps caused by keratin plugging hair follicles, and it affects roughly up to 40% of adults and a higher percentage of teens. I tell patients that consistent use of gentle exfoliants-urea, lactic acid, or low-strength retinoids-often improves texture, while moisturization helps reduce seasonal flares.
In my experience KP is strongly genetic, worse with dry skin and in winter, and can take 6-12 weeks to respond to therapy; for stubborn cases I consider in-office options like microdermabrasion or fractional laser. A practical regimen I use combines nightly chemical exfoliation (eg, lactic acid 5-12%) with twice-daily emollients containing 5-10% urea, which many patients report reduces roughness and redness within two months.
When to Seek Professional Help
If bumps persist beyond 6 weeks, worsen despite OTC care, or cause pain and visible scarring, I recommend seeing a clinician. In my practice I treat rapid spread, fever, intense pain, or bleeding as signals to seek care within days. For stubborn but less severe issues, a dermatology visit within 4-8 weeks often prevents permanent pits and identifies targeted therapies.
Signs of Serious Conditions
You should act when lesions are deep nodules >5 mm, recurrent cysts that leave pits, or eruptions accompanied by fever or swollen lymph nodes. I find immunosuppressed patients and those with >20 new lesions in a week more likely to have bacterial or viral complications. Ulceration, rapid enlargement, or persistent bleeding usually prompt biopsy and urgent treatment to exclude malignancy or aggressive infection.
Consultation with Dermatologists
When you consult a dermatologist I take a focused history, perform dermoscopic and clinical exams, and order tests such as KOH preps, bacterial swabs, or a punch biopsy when needed. Treatments range from topical retinoids and oral antibiotics to intralesional steroids, cryotherapy, laser, or isotretinoin (commonly 0.5-1 mg/kg/day) for nodulocystic disease.
Bring photos showing progression, a list of current medications (including any steroids or hormones), and previous treatment attempts; I use baseline photos to track response. Typical improvement appears in 4-12 weeks for most therapies, while isotretinoin courses often run 4-6 months. Discuss contraception, monitoring labs, and strategies to minimize scarring and recurrence.
Treatment Options
I prioritize a stepwise plan based on lesion type and severity: start with gentle cleansers and targeted topicals, escalate to combination therapy if comedones or inflammatory bumps persist, and refer after 6-12 weeks or sooner for worsening, pain, or scarring. In practice I combine keratolytics, antimicrobials, and retinoids to address clogged pores, bacteria, and abnormal keratinization.
Over-the-Counter Solutions
I recommend evidence-backed OTCs: salicylic acid (0.5-2%) for follicular exfoliation, benzoyl peroxide (2.5-10%) to reduce P. acnes, and OTC adapalene 0.1% to normalize cell turnover. Use benzoyl peroxide nightly or with adapalene for synergy; expect visible improvement in 6-12 weeks, and stop if you develop severe irritation or allergic symptoms.
Prescription Treatments
I reserve prescription options for persistent or inflammatory lesions: topical retinoids like tretinoin (0.025-0.1%) or tazarotene, azelaic acid 15-20%, topical clindamycin, and oral agents such as doxycycline (50-100 mg). For hormonal flares I may suggest combined oral contraceptives or spironolactone (50-200 mg). Oral isotretinoin is for resistant nodulocystic disease and requires lab monitoring.
In practice I pair topical retinoids with benzoyl peroxide to lower antibiotic resistance and usually limit oral doxycycline to about 3 months. I counsel on side effects: retinoids cause dryness and photosensitivity, spironolactone can affect blood pressure and electrolytes, and isotretinoin is teratogenic, requiring monthly pregnancy tests and liver/lipid monitoring.
Preventative Measures
I focus on consistent daily care and targeted habits that lower recurrence: use non‑comedogenic products and wear SPF 30+ daily, cleanse twice a day with a gentle cleanser, exfoliate with a BHA (salicylic acid 0.5-2%) 1-2 times weekly, and introduce a topical retinoid like adapalene 0.1% gradually to normalize keratinization and reduce comedones.
Skincare Routines
I recommend a simple, evidence‑based routine: cleanse twice daily, apply benzoyl peroxide 2.5-5% to inflammatory lesions, and use salicylic acid (0.5-2%) for clogged pores. Follow with a non‑comedogenic moisturizer to protect the barrier and use oil‑free, SPF‑rated makeup. Avoid abrasive scrubs and patch‑test new actives, increasing frequency over 4-8 weeks to limit irritation.
Lifestyle Changes
I advise small habit shifts that make a measurable difference: cut back on high‑glycemic foods and limit skim milk intake, manage stress, aim for 7-9 hours sleep, and shower within 30 minutes after sweating. Also avoid touching your face and launder pillowcases at least twice weekly to reduce transfer of oil and bacteria.
Several studies and clinical observations support these steps: randomized trials report lesion reductions of roughly 20-50% over 8-12 weeks with a low‑glycemic diet, and observational data link skim milk to higher acne prevalence. I also use practical measures-30‑minute post‑exercise cleansing, switching to silk or cotton pillowcases, and short daily stress practices (5-10 minutes breathing or mindfulness)-to lower flare frequency without immediately escalating to prescription therapy.
Conclusion
To wrap up, I explain that those little bumps on your forehead or cheeks most often result from clogged pores, excess oil, acne, milia, irritation, or allergic and heat-related reactions; noting their appearance and triggers helps me guide you toward gentle cleansing, appropriate topical options, or a dermatologist visit if they persist or worsen.
FAQ
Q: What common conditions cause little bumps on the forehead or cheeks?
A: The most common causes are closed comedones (whiteheads) and open comedones (blackheads) from acne; milia (tiny keratin-filled cysts); sebaceous hyperplasia (enlarged oil glands); folliculitis (inflamed hair follicles); and rosacea or perioral dermatitis in some people. Distribution, color, texture, itch or pain, and whether they recur help distinguish them.
Q: How can I tell a whitehead from milia?
A: Whiteheads are comedones with trapped oil and dead skin that can become inflamed and respond to acne treatments (salicylic acid, benzoyl peroxide, topical retinoids). Milia are firm, pearly, keratin-filled cysts that don’t open easily and often need professional extraction or topical retinoids and gentle exfoliation for improvement.
Q: Could these bumps be sebaceous hyperplasia, syringomas, or early rosacea?
A: Yes. Sebaceous hyperplasia are soft, yellowish, domed bumps with a central dell, common in adults with oily skin. Syringomas are small, flesh-colored papules (often around the eyes). Rosacea causes persistent redness with papules and pustules and usually includes flushing. A dermatologist can identify and treat these specifically (electrosurgery, laser, prescription topicals).
Q: Can hair products, sweat, or masks cause these bumps?
A: Yes-pomade acne, mask-related acne (maskne), and clogged pores from heavy oils or silicones can cause forehead and cheek bumps. Sweat and friction can worsen them. Switching to non-comedogenic, water-based products, cleansing after sweating, and reducing occlusive cosmetics typically helps.
Q: What about itchy, uniform small bumps-could that be fungal acne or bacterial folliculitis?
A: Fungal folliculitis (Malassezia) causes itchy, uniform small pustules or papules, commonly on the chest and back but also on the face; it responds to topical/oral antifungals (ketoconazole, fluconazole). Bacterial folliculitis produces inflamed pustules and soreness and may need topical or oral antibiotics. A clinician can confirm the cause and tailor treatment.
Q: What home care and over-the-counter options help these bumps, and should I pop them?
A: Avoid popping or aggressive squeezing. Use gentle cleansers, oil-free moisturizers, sunscreen, and targeted OTC actives: salicylic acid to exfoliate follicles, benzoyl peroxide for bacteria/reduction of inflammation, and topical retinoids to normalize cell turnover. Warm compresses can ease inflammatory lesions. If using multiple actives, introduce slowly to limit irritation.
Q: When should I see a dermatologist about forehead or cheek bumps?
A: See a dermatologist if bumps are persistent despite OTC care, painful, spreading, recur repeatedly, cause scarring or pigment changes, are itchy and not responding to antifungals or antibiotics, or if diagnosis is unclear. A dermatologist can biopsy, perform extractions, prescribe stronger topical/oral meds, or offer procedures (chemical peels, lasers, light therapy, surgical removal).