You may notice persistent dark spots, and I explain why hyperpigmentation is especially common in darker skin tones. I describe causes-post-inflammatory hyperpigmentation, melasma, hormonal shifts, and sun exposure-and show how unprotected sun exposure and aggressive treatments can worsen pigmentation or cause scarring. I outline evidence-based options like topical retinoids, azelaic acid, and supervised peels, and stress that consistent sun protection and tailored professional care yield the best outcomes for your skin.
Key Takeaways:
- Hyperpigmentation in darker skin commonly results from excess melanin triggered by inflammation (post-inflammatory hyperpigmentation), hormonal changes (melasma), sun exposure, acne, or trauma.
- Inflammation and skin injury are major drivers-picking, harsh treatments, or irritation often worsen or prolong pigmentation.
- Daily broad-spectrum sun protection (SPF 30+, physical blockers like zinc oxide or titanium dioxide) is foundational to prevent and treat pigmentation.
- First-line topicals: hydroquinone (short-term, supervised), azelaic acid, niacinamide, kojic acid and low-strength retinoids-use with sunscreen and gentle skincare to minimize irritation.
- Procedural options (superficial chemical peels, microneedling, low-fluence/non-ablative lasers) can help but must be performed by experienced clinicians; aggressive lasers/peels risk worsening pigmentation.
- Avoid unregulated skin-lightening agents (steroids, mercury), patch-test new treatments, and stop any product that causes irritation or increased darkening.
- Improvement is gradual (weeks-months); address underlying triggers (acne, hormonal factors) and consult a dermatologist for individualized combination therapy.
What is Hyperpigmentation?
Definition and Types
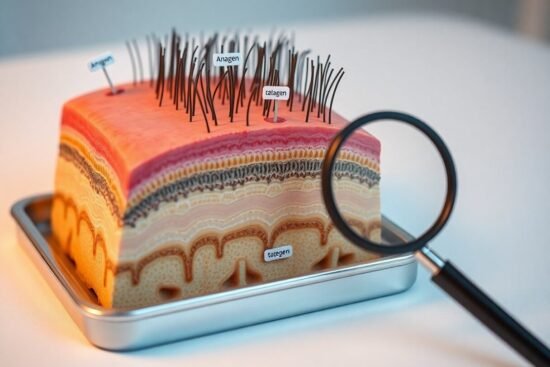
I define hyperpigmentation as localized darkening from excess melanin after inflammation, hormones, or UV exposure. In darker skin I commonly see three patterns: post‑inflammatory hyperpigmentation (PIH), melasma, and solar lentigines, each differing by depth and trigger. I note PIH often follows acne or trauma and can persist for months. The mechanisms involve increased melanocyte activity and dermal melanin deposition.
- Post‑inflammatory hyperpigmentation (PIH)
- Melasma
- Solar lentigines
- Drug‑induced hyperpigmentation
| Post‑inflammatory hyperpigmentation (PIH) | Dark macules after acne, eczema, trauma; often epidermal or mixed depth |
| Melasma | Symmetric facial patches tied to hormones and UV; common in women |
| Solar lentigines | Sun‑related, well‑defined brown spots; cumulative UV exposure |
| Drug‑induced | Medications (e.g., antimalarials, antibiotics) causing diffuse or patchy pigment |
| Nevus of Ota | Unilateral bluish facial/ocular pigmentation present from adolescence or earlier |
Prevalence in Darker Skin Tones
I see PIH in up to 60-70% of acne patients with Fitzpatrick IV-VI in clinic series, while melasma prevalence ranges from about 5-15% in high‑risk groups such as pregnant women or those on hormonal contraception. You’ll notice PIH often persists 3-12 months and can recur after new inflammation. I emphasize that darker skin shows more pronounced, longer‑lasting pigmentation compared with lighter skin.
I’ve treated cohorts where darker‑skinned patients report greater psychosocial impact; in one audit 58% ranked pigmentation as their top cosmetic concern. I advocate stepwise management: topical retinoids, azelaic acid, and supervised short‑course hydroquinone accelerate fading, whereas aggressive lasers or deep peels carry a high risk of worsening PIH. You should plan for months of therapy plus ongoing photoprotection and maintenance to reduce relapse.
Causes of Hyperpigmentation
I identify multiple interacting causes: genetic predisposition, inflammation from acne or eczema, hormonal shifts (pregnancy, contraceptives), sun and visible light, friction, and certain medications; in darker phototypes (Fitzpatrick IV-VI) post-inflammatory hyperpigmentation occurs in many clinical series, often after acne or dermatitis, and UV exposure amplifies existing spots within weeks, so I prioritize targeted prevention and tailored treatment plans for your risk profile.
Genetic Factors
I find that inherited differences in melanogenesis shape baseline pigmentation and reactivity, with gene variants altering melanin type, enzyme activity, and melanocyte responsiveness.
- MC1R – modifies eumelanin/phaeomelanin balance
- TYR – controls tyrosinase activity
- Melanocyte density – affects response to injury
Perceiving your family history and ethnic background helps me predict your susceptibility and guide prevention strategies.
Environmental Triggers
I see sun and external factors as common catalysts: daily UVA and visible light increase melanin synthesis, while air pollution and heat amplify inflammation; for example, visible light can worsen pigmentary disorders in darker skin and urban studies link particulate exposure to higher facial pigmentation, so practical photoprotection is central to management.
I expand on triggers by noting mechanisms and examples: UVA/UVB activate tyrosinase and generate reactive oxygen species, visible light induces long-lasting pigment via opsin pathways, and pollutants (PM2.5) promote oxidative stress and cytokine release. Friction from clothing or shaving produces localized post-inflammatory hyperpigmentation, and certain procedures (deep peels, nonselective lasers) carry a 10-30% risk of worsening pigment in darker skin if not calibrated. I therefore favor broad-spectrum SPF 30+, physical blockers and tinted sunscreens with iron oxide, plus gentle exfoliation and anti-inflammatory strategies to limit environmental-driven pigmentation.
Common Types of Hyperpigmentation
I classify the most frequent patterns in darker skin as distinct clinical entities that change treatment choice: melasma, post-inflammatory hyperpigmentation, solar lentigines, periorbital hyperpigmentation, and guttate macular hyperpigmentation. These differ by trigger, distribution, and response to therapy-PIH often follows acne while melasma links to hormones and sun. Knowing the dominant type directs whether I prioritize sun protection, topical agents, or procedural caution.
- Melasma
- Post-Inflammatory Hyperpigmentation
- Solar Lentigines
- Periorbital Hyperpigmentation
- Guttate Macular Hyperpigmentation
| Melasma | Hormonal link, centrofacial distribution; worsens with UV exposure; common in pregnancy. |
| Post-Inflammatory Hyperpigmentation | Follows acne, eczema, trauma; variable fade (often 3-12 months); frequent in Fitzpatrick IV-VI. |
| Solar Lentigines | Sun-induced, well-demarcated brown spots in older adults; procedural options exist but require caution. |
| Periorbital Hyperpigmentation | Multifactorial (genetics, thin skin, vascular or pigmentary causes); often resistant and needs multi-modal approach. |
| Guttate Macular Hyperpigmentation | Small, scattered macules often on trunk/extremities; consider medication or metabolic triggers. |
Melasma
I see melasma as symmetric brown patches on the cheeks, forehead and upper lip; it’s strongly linked to hormonal shifts and affects up to 50% of women in some pregnancy series. Sun exposure amplifies lesions and reduces treatment response, so I emphasize daily broad‑spectrum sunscreen and, when indicated, supervised topical regimens such as azelaic acid, tranexamic acid, or a triple combination.
Post-Inflammatory Hyperpigmentation
You often find PIH after acne, eczema, insect bites, or procedures; I note it can take 3-12 months to fade naturally and sometimes longer without intervention. Early, gentle treatment with topical retinoids, azelaic acid, or low‑strength hydroquinone can speed resolution, while aggressive therapies may worsen pigment if inflammation persists.
In my practice I link PIH severity to inflammation depth: epidermal PIH responds faster, dermal pigment is more persistent and may need combination therapy. I avoid aggressive resurfacing on active inflammation because procedures carry a higher risk of aggravating pigmentation in Fitzpatrick IV-VI skin. I prioritize strict sun protection, anti‑inflammatory control, and stepwise escalation-adding chemical peels, fractional lasers, or oral tranexamic acid only when benefits outweigh the heightened risk of rebound hyperpigmentation.
Diagnosis of Hyperpigmentation
I approach diagnosis by mapping lesion pattern, onset, triggers, and treatment history, noting whether pigmentation follows inflammation, hormones, or drugs; in Fitzpatrick IV-VI skin I pay particular attention to post-inflammatory patterns after acne or procedures. I document progression with serial photos and prioritize tests that separate epidermal from dermal causes because accurate classification directly determines effective therapy.
Visual Examination
I inspect lesions in natural and magnified light, assessing color, border sharpness, and distribution-epidermal pigment is warm brown and often sharp, while dermal gives a blue-gray cast. I check for accompanying signs like active acne, scarring, or scale and record any asymmetry or rapid change; using clinical photography at baseline and 6-12 week intervals helps you and me track response objectively.
Dermatological Assessments
I use adjunct tools: Wood’s lamp (UVA ~365 nm) to accentuate epidermal pigment, dermatoscopy at 10x-20x to evaluate melanin granularity and perifollicular involvement, and targeted punch biopsy when atypia or diagnostic uncertainty exists. I also order labs-pregnancy test, TSH, cortisol-when hormonal drivers are suspected. Biopsy is uncommon but decisive when malignancy or unusual inflammation is a concern.
I often choose management after these assessments; for example, if Wood’s lamp shows epidermal accentuation I favor topical hydroquinone, retinoids, and strict photoprotection, whereas dermal pigmentation prompts avoidance of aggressive resurfacing lasers. In one typical case I switched from ablative laser to topical combination therapy after dermoscopy revealed deep melanin, preventing possible worsening-matching treatment depth to pigment depth markedly improves outcomes.
Treatment Options
I favor a multi-modal plan combining topical agents, in-office procedures, and strict sun protection; for many patients I see, combination therapy yields 50-70% improvement within 3-6 months. I warn you that aggressive treatments can provoke post-inflammatory hyperpigmentation, so sequencing, test spots and gentle protocols matter.
Topical Treatments
I use targeted actives-hydroquinone (2-4%), azelaic acid (15-20%), topical tranexamic acid, retinoids, and vitamin C-in stepped regimens; expect visible change after 8-12 weeks. I advise nightly retinoid rotation, short-term hydroquinone cycles to reduce ochronosis risk, and daily SPF 30+ to protect results.
Professional Procedures
I recommend superficial chemical peels (20-35% glycolic, 30% salicylic), microneedling (3-6 sessions, 4-6 weeks apart), and low-fluence Q-switched Nd:YAG (1064 nm) for darker skin; these balance efficacy with lower PIH risk, but you should expect multiple sessions and ongoing maintenance.
Before lasers or peels I precondition skin with topical agents (4% hydroquinone or azelaic acid for 4-6 weeks) and always perform a test spot; I require experienced providers because improper settings frequently cause recalcitrant PIH. For perspective, microneedling trials report ~30-50% pigment reduction after three sessions, and per-session costs generally range from $200-$1,200 depending on modality and location.
Prevention Strategies
I focus prevention on stopping triggers that drive melanin overproduction: limit inflammation from acne or shaving, control hormonal flares when feasible, and enforce strict photoprotection; PIH can persist for months to years in darker skin, so early behavior change plus targeted topicals lowers incidence. I coach patients to avoid picking, use non-comedogenic moisturizers with ceramides, and follow follow-up plans to catch recurrence quickly.
Sun Protection
For sun protection I prescribe a broad-spectrum sunscreen of at least SPF 30+ every morning and reapplication every two hours when outdoors; I favor physical filters (zinc oxide/titanium dioxide) for lower irritation and recommend UPF clothing, wide-brim hats, and timing outings around peak UV (10:00-16:00). In my experience, consistent sunscreen use halves the risk of PIH darkening after procedures or acne flares.
Skincare Routines
I design routines around gentle cleansing (pH-balanced), daily sunscreen, and targeted actives such as azelaic acid (15-20%), niacinamide (4-5%), and nightly retinoids titrated slowly; I avoid high-concentration exfoliants initially to prevent irritation, and I advise patch testing new products to protect against inflammatory rebound in darker skin.
I often provide a practical regimen: morning-gentle cleanser, vitamin C (10-20%) if tolerated, moisturizer, SPF 30+; night-cleanser, azelaic acid or topical brightener, retinoid 2-3 nights/week building to nightly, then moisturizer. I limit hydroquinone to monitored courses (commonly up to 3 months) and arrange in-office peels or laser only with experienced providers to reduce risk of paradoxical hyperpigmentation; professional supervision is necessary.
Summing up
Upon reflecting, I summarize that hyperpigmentation in darker skin stems from melanin overproduction triggered by sun exposure, hormones and inflammation; I stress that you can manage it safely with consistent sun protection, gentle topical lighteners (retinoids, vitamin C, azelaic acid or supervised hydroquinone), and conservative procedures tailored to your skin type, while avoiding aggressive treatments that increase risk of worsening pigment; I recommend working with a knowledgeable clinician to design a personalized, long‑term plan for your skin.
FAQ
Q: What is hyperpigmentation and why does it often appear differently on darker skin tones?
A: Hyperpigmentation is excess melanin production or uneven melanin distribution that creates darker patches. In darker skin, melanosomes are larger and more densely distributed, so inflammatory triggers (acne, cuts, eczema) more readily lead to post-inflammatory hyperpigmentation (PIH) that appears darker and can persist longer than in lighter skin.
Q: What are the most common causes of hyperpigmentation in people with darker skin?
A: Frequent causes include PIH from acne, trauma, or inflammatory skin conditions; melasma related to hormones or birth control; sun-induced lentigines; medication- or chemical-induced pigmentation; and scarring or burns. Genetic predisposition and repeated irritation from hair removal or aggressive treatments also increase risk.
Q: How can I reduce the risk of developing PIH after skin injury or acne?
A: Treat inflammation early with appropriate acne or dermatitis therapies, avoid picking or squeezing lesions, use gentle non-irritating cleansers and moisturizers, apply broad-spectrum sunscreen daily (SPF 30+), wear protective clothing, choose gentle hair-removal methods, and consult a clinician before trying strong peels or lasers.
Q: Which topical treatments are effective and safe for darker skin tones?
A: Effective options include azelaic acid, niacinamide, topical retinoids, vitamin C, tranexamic acid, mandelic acid, and short courses of hydroquinone under supervision (usually 2-4%). Combinations (e.g., retinoid + hydroquinone + sunscreen) often work better. Start slowly, monitor for irritation, and patch-test products to avoid treatment-induced hyperpigmentation.
Q: Are in-office procedures like peels and lasers safe for darker skin?
A: They can be safe when chosen and performed by experienced providers using conservative settings. Superficial chemical peels (mandelic, lactic) and microneedling are often lower risk. Lasers require selection of wavelengths and parameters suited to higher melanin (for example, 1064 nm Nd:YAG at low fluence) and may still carry PIH risk. Pre- and post-treatment topical preparation and strict sun protection reduce complications.
Q: How long does it usually take to see improvement in hyperpigmentation?
A: Topical agents typically require 8-12 weeks to show initial change and 3-6 months for more pronounced improvement. In-office treatments may accelerate results but often need multiple sessions spaced weeks apart. Maintenance therapy and sun protection are necessary to prevent recurrence.
Q: When should I consult a dermatologist for hyperpigmentation?
A: See a dermatologist if patches are widespread, rapidly changing, painful, bleeding, unresponsive to OTC measures after several months, or if the diagnosis is uncertain. A clinician can confirm the cause, prescribe stronger or combination therapies, recommend safe procedures, and create a monitoring plan to minimize side effects and PIH risk.